PURPOSE
- This guideline serves as recommendations to the care team for consideration when to prone. If proning is decided as part of the treatment plan by the attending intensivist, this guideline provides a standard operating procedure for proning.
- The purpose of prone positioning is to improve the oxygenation status of critically ill patients with severe acute respiratory distress syndrome (ARDS).
- Prone positioning improves both oxygenation and more importantly mortality in patients with severe ARDS.
- The earlier the prone positioning commences the better the possible outcomes (recommended within the first 36 hours of illness).
- Eligibility/Contraindications
- Eligibility
- Severe ARDS with severe hypoxemia (P/F ratio ≤ 150 mmHg on ≥FiO2 .60 with PEEP ≥ 5) not responding to Low Tidal Volume Ventilation (LTVV) as an initial strategy
- Approval of intensivist in collaboration with nursing and respiratory therapy based on patient assessment
- Patients with Severe ARDS not responding to LTVV
- Early Severe ARDS presentation
- Hemodynamically stable on current vasopressor and oxygen requirements
- Absolute Contraindications
- Patients with unstable fractures of cervical, spine, pelvis, face, ribs, femur
- Intracranial hypertension >30 mmHg
- Relative Contraindications
- Uncleared cervical spines: Patients with radiologically clear cervical spines may be proned if cervical immobilization can be maintained.
- Pregnancy: Consult OB-GYN
- Life threatening arrhythmias
- Ventral burns or open wounds of face, abdomen, chest: Patients with open abdomens and a vacuum dressing may be proned after evaluation of the dressing for intact condition. An abdominal binder may be added for extra support.
- Facial or tracheal surgery or facial trauma within the last 15 days
- Sternotomy < 7 days
- Tracheostomy < 7 days old: Consult ENT/Surgery for airway stability
- Pacer/ICD placed within the last 2 days
- Hemodynamic instability despite appropriate pressors
- Adequate analgesia/sedation/paralysis as needed to achieve passive ventilation
- Active peritoneal dialysis
- Single anterior chest tube with air leak
- Uncontrolled hemorrhage
- Intra-abdominal hypertension with intra-abdominal pressure > 20mmHg
- Other conditions to consider: intestinal ischemia, known difficult airway, recent abdominal incision/surgery, recent breast implants, penile prosthesis
II. Procedure
- Family Education
- Explain to the family the purpose of prone positioning.
- Explain the process of placing the patient prone.
- Instruct family about the facial edema and tissue injury that may occur after proning and provide emotional support as needed.
- Preparation
- Patient Assessment
- Assess the patient prior to initiating treatment. Document the position of the endotracheal tube at lip (or mouth), invasive lines, ventilator settings, last arterial blood gas (ABG) with P/F ratio calculation, physical assessment, skin condition and hemodynamic profile.
- Analgesia/Sedation and Neuromuscular Blockade: Aggressive pain and anxiety control is essential for the position change to be effective. Collaborate with the ICU team (provider, pharmacist and respiratory therapist) to insure adequate analgesia and sedation prior to proning the patient. The need for chemical paralysis is more than likely necessary. Use appropriate rating scales to assess such as RASS (for sedation), BIS monitoring (for sedation), Train of Four (adequacy of paralysis).
- Assess for adequate VTE prophylaxis.
- Plan ahead for anticipated procedures such as imaging, blood draws, and any off-unit testing.
- Plan of Care
- Goals of proning should be clearly identified by every member of treatment team: providers, RNs, respiratory therapists, occupational therapy, or physical therapy
- Goals of proning treatment includes the following measures:
- FiO2/PEEP weaning goals
- PaO2 and arterial oxygen saturation (SaO2)
- Duration of prone position. Current recommendation is 16-18 hours but may be utilized up to 20 hours per day
- Gather supplies included in Proning Kit
- AP for foam placement
- Z-flo head positioner
- Foam bolster pillow
- Comfort glide sheet
- Comfort glide absorbent pad
- 2 sure prep no sting swabs (3ml)
- 1 Optifoam thin
- 4 Optifoam gentle light 3×3
- 4 Optifoam bordered SA 6×6
- 4 Optifoam bordered SA 4×4
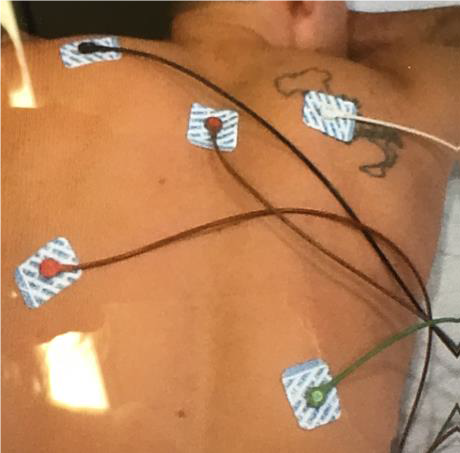
- 5 ECG electrodes
- 1 roll paper tape
- Obtain additional supplies equipment
- 6 pillows
- Lubricant for the eyes (gently taped closed is optional)
- Clean linen for bed assembly.
Supply placement for wound prevention when prone
| Description | Manufacturer | Item # | Placement guidance |
| 2 sure prep no sting swabs 3ml | Medline | 955606 | Forehead, cheeks, chin, dorsal toes |
| 1 Optifoam thin | Medline | 926253 | Under devices |
| 4 Optifoam gentle light 3×3 | Medline | 953445 | Forehead, cheeks, chin |
| 2 Optifoam bordered SA 6×6 | Medline | 982123 | Hips, chest |
| 4 Optifoam bordered SA 4×4 | Medline | 958424 | Knees, shoulders |
| Foam Bolster pillow | Medline | 23962 | Feet offloading |
| Z-flo | Molnlyke | 213423 | Head rest with ETT |
| Comfort glide sheet | Medline | 901648 | Proning tool |
| Comfort glide absorbent pad | Medline | 923968 | Use with above |
| 5 ECG electrodes | Medline | 150836 | ECG monitoring |
| 1 roll paper tape | Medline | 63830 | Eye protection |
- Prepare patient while in supine position. Cluster care when patient is in isolation:
- Consider a wound nurse consult
- Reposition and secure all lines, tubes, and drains
- Apply necessary dressings for protection,
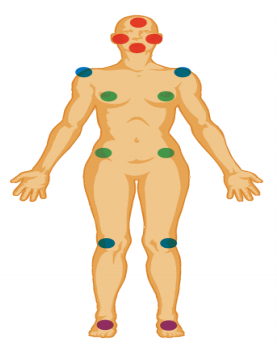
- Place ECG electrodes on back when prone
- Max-inflate the mattress
- Eyes taped closed horizontally
- Daily hygiene is completed, i.e., mouthcare, bathing, emptying/changing of stoma bags, etc.
- Verify patent in-line suctioning
- Verify OGT/DHT placement, which ideally should bepost pyloric. Turn tube feedings off for a minimum of 1 hour prior to proning.
- Secure airway. Tape oral endotracheal tube (ETT) circumferentially around the head to protect against tube dislodgment from increased oral and nasal secretions or use an ETT holder.
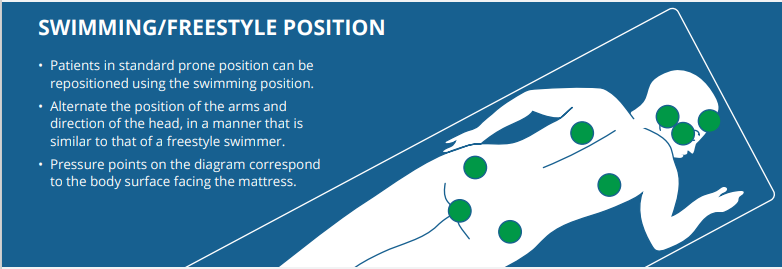
- Reposition arms and head every 2 hours when in prone position
- Ensure emergency airway and resuscitation equipment is immediately accessible.
Image of EKG placement in prone position
III. IMPLEMENTATION
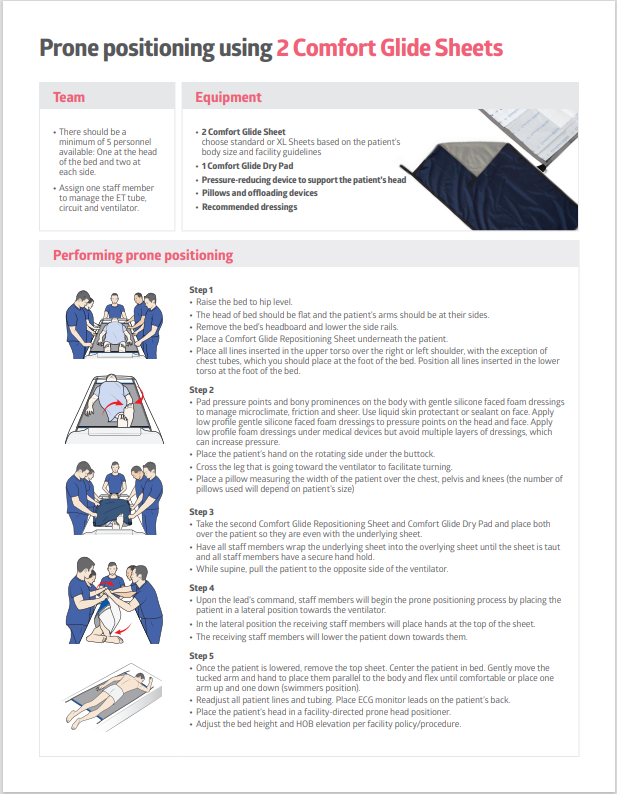
- Decide as a team to prone manually or with a mechanical proning bed. Manual proning is the preferred method where possible.
- Assemble a four- to six-person team.
- Procedure coordinator (1): delegates responsibility (usually primary ICU RN or charge RN)
- Airway monitor (1): respiratory therapist
- “Flippers” (1 or 2): located on side of bed and turns patient towards catcher
- “Catchers” (1 or 2): located on opposite side of bed and receives the turning patient
- Use the 2 Comfort Glide Sheet Directions below for manual proning
IV. CLINICAL ASSESSMENT – POST PRONATION
- Assessment steps for a safe and successful pronation
- Check all pressure areas.
- Ensure no tubing or cables are trapped and are transferred to the respective sides of the bed.
- Ensure patient’s tongue is in his/her mouth—if tongue is swollen or protruding, use bite block or oropharyngeal airway.
- Be sure to monitor patient’s position during turning—shoulders are at high risk for dislocation
- If patient is paralyzed, utilize Train of Four.
- BIS monitoring should be utilized for sedation.
- Pillows
- Are pillows positioned appropriately for offloading?
- Are feet elevated?
- Head, Tubes & Lines
- Are ET/NG/IV tubes kink free and in correct positioning?
- Is patient’s head positioned appropriately?
- Ventilation OK?
- IV medications restarted if necessary?
- Arms
- Positioning: no over extension and no pressure on pressure points?
- Other things to remember:
- If at any time there is an issue during the turn, verbalize for the team to STOP.
- Silk tape should be used for ETT securement.
- Reposition every 2 hours: Turn head and ensure raised arm position changed.

IV. MONITORING AND EVALUATION
A. Ongoing Patient Assessment and Care
- Assess the patient post-procedure for tolerance of prone positioning, including stabilized or improved oxygenation and hemodynamic stability:
- Respiratory rate and effort
- Continuous Pulse Oximetry (SpO2)
- ABG to calculate PaO2/FiO2 ratio 1-4 hours post-proning
- Poor tolerance of prone positioning is indicated by hemodynamic and oxygenation parameters that deteriorate once proned and do not stabilize within 10 minutes after the turn.
- Positive patient response to therapy is defined by an improvement in oxygenation parameters.
- When feasible, assess for “sedation vacation” and if appropriate “spontaneous awakening trial” daily.
- Ensure proper body alignment, tube and catheter patency. Rehab Medicine Therapy staff to assist/lead positioning
- Use splints or roll as well as heel boots to prevent foot drop.
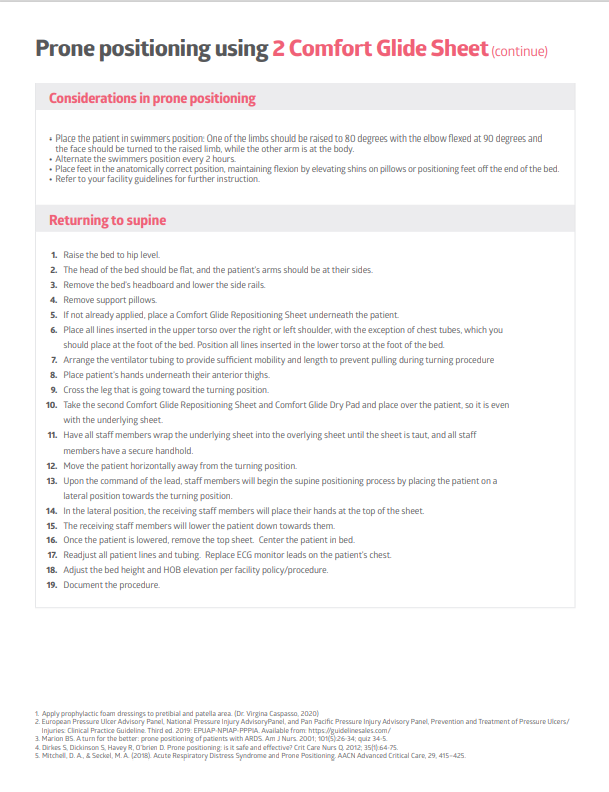
- Reposition arms and head every two hours or as tolerated. Head turning is done to prevent compression of the eyes and pressure ulcers.
- Arms are in the “swimmer’s position”: one arm is parallel to the side of the body and the opposite arm is bent at elbow with the hand near the ear. Note: shoulder should not be hyperextended above head due to risk for brachial plexus injury.
- Patient head should be turned towards elevated upper extremity.
- When positioning a patient’s upper extremities, complete gentle ROM/abduction until resistance is felt, then back off by 5-10 degrees of motion. A patient should not be left in their absolute MAXIMUM range of motion for prolonged periods.
- If not using Tortoise Prone Turn Assist Device, pelvic roll should not compress penis or scrotum and chest roll should not compress breast.
- Assess and intervene to prevent potential complications, including:
- Unplanned extubation
- Tube and catheter dislodgment
- Pressure injuries
- Nerve injury
- Eye damage
- Hemodynamic changes
- Collaborate with provider regarding length of time the patient will remain prone. It is recommended for patients to be proned for a minimum of 16-18 hours a day, but this may be adjusted based on patient tolerance. Daily or more frequent assessment of need to continue proning should be assessed and documented.
- To turn the patient to the supine position, repeat the appropriate preparation and procedure steps.
B. Indications to discontinue proning therapy
- Improved oxygenation: Improvement of PaO2/FiO2 to > 150 with FiO2 ≤ 0.60 and peep ≤ 10 cm H2O
- Ineffectiveness: Prone PaO2/FiO2 > 20% lower than pre-prone PaO2/FiO2 in 2 consecutive proning sessions
- Complications (discontinue immediately):
- Unplanned extubation
- ETT obstruction
- Main stem intubation
- Massive hemoptysis
- SpO2 < 85% or PaO2 < 55 for more than 5 minutes while on FiO2 100%
- Sustained bradycardia <30 BPM for a minute
- SBP < 60 for more than 5 minutes
- Cardiac arrest
- Clinically significant pneumothorax
- Any other life-threatening complication
- Code status downgraded. Discuss with managing team and family goals of proning and plan of care.
V. DOCUMENTATION
A. Ensure that the following data/information are documented in Epic
- Position of the endotracheal tube prior to proning, when prone, and when returned to supine.
- Ventilator settings
- ABGs
- Physical assessment
- Skin condition
- Hemodynamic profile
- Pain using an appropriate rating scale
- Sedation using an appropriate rating scale
- Tolerance of prone positioning, including all vital signs and hemodynamic profile
VI. Resources
- Elsevier Skills: Pronation Therapy – CE
- Uptodate.com : Prone ventilation for adult patients with acute respiratory distress syndrome, https://www.uptodate.com/contents/prone-ventilation-for-adult-patients-with-acute-respiratory-distress-syndrome?search=prone%20positioning&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H4007302505
REFERENCES
Bein, T., Grasso, S., Moerer, O., Quintel, M., Guerin, C., Deja, M., … Mehta, S. (2016). The standard of care of patients with ARDS: ventilator settings and rescue therapies for refractory hypoxemia, Intensive Care Medicine, 42, 699-711.
Bloomfield, R., Noble, D.W., & Sudlow, A. (2015). Prone position for acute respiratory failure in adults (review). Cochrane Database of Systematic Reviews 2015 (11). doi:10.1002/14651858.CD008095.pub2
Drahnak, D.M., & Custer, N. (2015). Prone positioning of patients with acute respiratory distress syndrome. Critical Care Nurse, 35(6), 29-37.
Fan, E., Del Sorbo, L., Goligher, E.C., Hodgson, C.L., Munshi, L., Walkey, A.J., … Brochard, L.J. (2017). An official american thoracic society/european society of intensive care medicine/society of critical care medicine clinical practice guideline: mechanical ventilation in adult patients with acute respiratory distress syndrome. American Journal of Respiratory Critical and Care Medicine, 195(9), 1253-1263.
Guerin, C., Reignier, J., Richard, J.C., Beuret, P., Gacouin, A., Boulain, T., … Ayzac, L. (2013). Prone positioning in severe acute respiratory distress syndrome. The New England Journal of Medicine; 368 (23), 2159-2168.
Hu, S.L., He, H.L., Pan, C., Liu, A.R., Liu, S.Q., Liu, L., … Qui, H.B. (2014). The effect of prone positioning on mortality in patients with acute respiratory distress syndrome: a meta-analysis of randomized controlled trials. Critical Care, 18, R109.
Lee, J.M., Bae, W., Lee, Y.J., & Cho, Y.J. (2014). The efficacy and safety of prone positional ventilation in acute respiratory distress syndrome: updated study-level meta-analysis of 11 randomized controlled trials. Critical Care Medicine, 42(5), 1252 – 1262.
Sud, S., Friedrich, J.O., Adhikari, N.K., Taccone, P., Mancebo, J., Polli, F., … Guerin, C. (2014). Effect of prone positioning during mechanical ventilation on mortality among patients with acute respiratory distress syndrome: a systematic review and meta-analysis. Canadian Medical Association Journal, 186 (10), E381-90. Vollman, K., Dickinson, S., & Powers, J. (2017). Pronation Therapy. In Wiegand, D. (Ed.), AACN Procedure Manual for High Acuity, Progressive and Critical Care, 7th Ed (142-163). St. Louis: Elsevier, Saunders.

